Authors:
Professor Hilali Noordeen1
Mr. Chadi Ali1
Mr. Naadir Nazar2
Institutions:
1Royal National Orthopaedic Hospital, Brockley Hill, Stanmore, United Kingdom
2University of Bristol, Bristol, United Kingdom
Introduction
Neuromuscular scoliosis (NMS) is the second most frequently encountered cause of scoliosis and presents a significant and complex clinical challenge with higher complications rates compared to patients with idiopathic scoliosis. NMS can be subclassified into neuropathic or myopathic causes and include conditions such as Cerebral palsy, Duchenne muscular dystrophy, Myelomeningocele, spinal muscular atrophy (SMA) and Fredrich ataxia, to name a few. It is also widely accepted that there may be overlap with congenital (e.g. spina bifida) and syndromic aetiologies. A scoliosis can present in any individual with a pre-existing neuromuscular diagnosis and can be further exacerbated if the patient is non-ambulant and wheelchair dependant. Muscular imbalance, discoordination and reduced head and trunk balance are shared features amongst most neuromuscular conditions. However, it is important to understand that it is difficult to generalise NMS into a single condition owing to the large number of underlying diagnoses and pathologies associated. While the orthopaedic manifestations of many of these patients may be similar, the nuances and complexity of the various underlying medical conditions makes each case unique and challenging.
The two main types of scoliosis, idiopathic and neuromuscular, are diagnosed when the curve present is greater than ten degrees. However, patients with NMS tend to develop long, sweeping S and or C – shaped curves that can involve the entire spine and sacrum – which is in stark contrast to idiopathic scoliosis where curves are generally restricted to smaller spinal segments. NMS curves are more likely to progress, and therefore this deformity presents a daily functional challenge to patients and families and impact on personal hygiene, sitting balance and skin integrity. These individuals also experience difficulties in daily care, positioning and ambulation. Pelvic imbalance can increase which results in a loss in sitting balance/positioning and the ability to sit independently. These serve as indications to begin and guide treatment.
Techniques
Non-operative management is indicated for some patients with early onset neuromuscular scoliosis (EOS). This can be sub-divided into congenital, infantile and juvenile groups and is defined as scoliosis seen anywhere before the age of nine. Conservative interventions include observation and wheelchair and seating modification which involve contouring the seating to their deformity. The next step involves wearing a firm moulded plastic brace around the upper body for a minimum of nineteen hours a day and can limit the worsening of the curvature during periods of growth. Some limitation of curve progression was shown by Olafsson et al whilst improvements in the curve angle was exhibited by Nakamura et. al in their studies of bracing in NMS patients. However, most studies generally find bracing to be ineffective with a limited effect on progression. It is instead primarily seen to support and improve sitting function as well as partially postpone the need for surgical intervention.
As the deformity progresses, pulmonary function can deteriorate owing to weak breathing muscles, the inability to clear secretions and the spinal deformity itself. Other vital organs may also be affected and include the cardiovascular, genito-urinary and gastroenterology systems. Surgical intervention is indicated when the curve continues to progress, resist conservative interventions and worsen sitting function. Through surgery the aim is to improve and maintain the patient’s (upright) posture, improve or restore sitting position/balance and prevent the decline of lung function and other vital organs. The hope is to provide the patient with the best functionality and quality of life.
Prior to any decision being made, a full pre-operative assessment is required to see if surgery can be safely undertaken. It involves a wide array of specialists taking a multi-disciplinary approach to obtain the best possible outcome. The benefits of surgical intervention are weighted against its difficulty and potential risk of complications in a risk-benefit analysis to make an informed decision. Using detailed information of the patient and their current condition, individuals are classified into three main groups: not for surgery, almost ready for surgery and ready for listing.
Surgery in neuromuscular scoliosis is more complex and requires long and extensive instrumentation. There are three main types which include magic rods, traditional growth rods and definitive spinal fusion. For early onset cases a MAGEC or traditional growth rod (TGR) can be considered once conservative options have been exhausted or if the curve has severely progressed. The aim of these growing rods is to maintain spinal growth during the rapid growth of a child and prevents the need for an early spinal fusion which can result in a short trunk and long limbs.
The TGR is a growth sparing technique that is currently the most common and desirable form of treatment for EOS. However, downsides exist and implantation of these TGR’s requires frequent open surgical distraction every six months to allow for growth. For instance, a 5-year-old girl will require around sixteen distractions if skeletal maturity is reached at thirteen years of age. These procedures are a particular issue for neuromuscular patients due to the high incidence of complications which include wound infection and restrictive lung disease. Some individuals may even be deemed too unfit for repeated anaesthesia. The complication rate seen can be as high as 19% whilst the overall wound complication rate increases by 24% for each procedure. Furthermore, a study by Noordeen et. al found that distraction forces significantly increase after repeated lengthening and the length obtained for each procedure exhibits a decreasing trend. There is also a need to consider the psychological and physiological effects of repeated surgery.
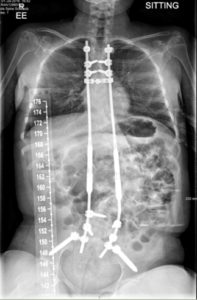

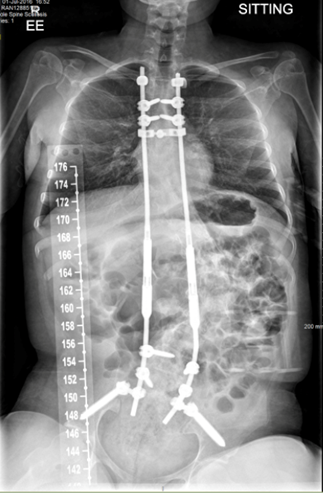
Figure 1- Bilateral MAGEC growth rod
For these reasons our practice recommends the use of the magnetic growth rods (MGR). We use T4 as the upper vertebral limit for instrumentation and in most cases the lower limit is at L4. The pelvis may be included if there is severe pelvic rotation. This decision is based on the individual case and the preference of the surgeon. The MGR system represents a relatively new technology which only requires an external, painless non-surgical distraction in the clinic or office setting with the patient awake throughout. It requires an electrically powered remote controller that utilises an electromagnetic field to distract and lengthen the spine. Several studies have explored the MGR and conclude that it shows very similar effectiveness for curve correction in comparison to the TGR. We authored a multi-centre study of EOS patients which showed the mean monthly T1–T12 and T1–S1 growths in MGR individuals were comparable with both normal growth and the growth achieved using the standard traditional growth rod. This technique also achieved and maintained a similar initial scoliosis angle correction when compared to the TGR. Similarly, a significant improvement in both pulmonary function (FVC, FEC1) and deformity correction was seen in a study of MGR treated patients with EOS secondary to neuromuscular disease (see article – oon, W. , Sedra, F. , Shah, S. , Wallis, C. , Muntoni, F. & Noordeen, H. (2014). Improvement of Pulmonary Function in Children With Early-Onset Scoliosis Using Magnetic Growth Rods. Spine, 39 (15), 1196-1202.).
Complications associated with MAGEC rods include their potential to break in early onset cases. If this occurs, we leave the rods in situ as the breakage itself does not cause any significant issues. If there is evidence of any complications or subsequent curve progression, we will then intervene. Furthermore, the electromagnetic field used for repeated distractions is not associated with any persistent or major side effects. Concerns have also arisen regarding the MGR’s potential to generate excessive metallic debris when these rods slide in the guiding fixtures. However, an analysis of our EOS patients exhibited that levels of aluminium and titanium in the blood were not clinically significant (see article – Borde, M. D., Sapare, S., Schutgens, E., Ali, C., & Noordeen, H. (2021). Analysis of serum levels of titanium and aluminium ions in patients with early onset scoliosis operated upon using the magnetic growing rod-a single centre study of 14 patients. Spine deformity, 9(5), 1473–1478.). Overall, the magnetic controlled growth rod presents a safe and effective modality to treat NMS whilst also allowing for spinal growth. In comparison to other methods, it is seen to have better long-term health gains and fewer complications while also providing a safe gradual correction of severe deformities in young individuals.

Figure 2 – Traditional growth rod
If the patient is more adult and closer to complete skeletal maturity, then definitive spinal fusion surgery is offered. As with other types of scoliosis, the goals of this surgery in NMS patients are to achieve a solid bony arthrodesis of the spine to correct the deformity, prevent further progression and restore overall standing or seating balance. Fusion balances the trunk in the frontal and sagittal planes and centres the head over the pelvis. A large proportion of NMS patients are non-ambulatory and therefore the fundamental aim is to create and maintain an upright posture. The surgical approach alongside the proximal and distal extent of the instrumentation and fusion are important technical considerations in this patient group. Most often a posterior spinal fusion approach is carried out due the long and extensive instrumentation and fusion needed for neuromuscular patients. Usually, we stop above at T4 to prevent conjunctional cervicothoracic kyphosis and fix down to no lower than L5. Once again, the pelvis may be included which is dependent on the degree of its displacement. The next question is whether to use a single or double rod. Dual rod segmental spinal instrumentation has been the standard surgical procedure for the management of NMS. This method has proven efficacy in achieving a solid arthrodesis and stabilizing the spine but has been associated with prolonged operative times, increased blood loss and infection. We performed a study of 28 consecutive neuromuscular scoliosis patients fused with a single corrective rod to evaluate its safety and efficacy. The results from this study indicate that unilateral instrumentation and fusion achieves satisfactory curve correction which is maintained at final follow up. Furthermore, we had significantly shorter volumes of intraoperative blood loss (675 ml) and operative times (196.6 minutes) as well as no cases of deep wound infection – all of which reduces patient morbidity. Careful preoperative patient preparation is also vital in reducing the rate of postoperative complications in this patient population. These findings are highly promising and justify a comparative analysis of the single rod verses the current standard dual rod technique.


Figure 3 – Single rod instrumentation & fusion

Figure 4 – Bilateral instrumentation and fusion
Complications & Conclusion
Scoliosis surgery has associated risks involved, some of which have been listed above. These risks are small but it is important that patients and their families are aware in order to have a clear understanding of the treatment being offered. Neuromuscular patients are at a higher risk of peri and post-operative complications due to underlying comorbidities, with the complication rate ranging from 18 – 75%. Deformities of the thoracic cage, aspiration issues, decreased mobility, inadequate nutrition status and cognitive impairment are some examples of comorbidities associated with an increased complication rate. Infection and metalwork breakage/failure are seen while neurological, gastrointestinal, respiratory, and spinal complications can also occur. Late post-operative complications include chronic infections, non-union, coccygeal pain, turning of the ribs (crankshaft phenomen) and implant-related issues.
An infection rate of 5.5% for NMS compared to 1.4% in adolescent idiopathic scoliosis (AIS) patients was reported by the Scoliosis Research Society Morbidity and Mortality Committee. Similarly, the new neurological deficit rate was 1.03% for neuromuscular patient’s vs 0.73% for AIS. (see article – Smith, J. S., Shaffrey, C. I., Sansur, C. A., Berven, S. H., Fu, K. M., Broadstone, P. A., Choma, T. J., Goytan, M. J., Noordeen, H. H., Knapp, D. R., Jr, Hart, R. A., Donaldson, W. F., 3rd, Polly, D. W., Jr, Perra, J. H., Boachie-Adjei, O., & Scoliosis Research Society Morbidity and Mortality Committee (2011). Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine, 36(7), 556–563).
Despite these issues, there are procedures we can implement to circumvent and treat most complications. A standardised preoperative evaluation should be carried out so that all risk factors are considered and dealt with appropriately. Respiratory rehabilitation and nutritional care are also important prior to intervention. For instance, pre- operative non-invasive ventilation (NIV) has been shown to strengthen respiratory muscles and reduce the rate of complications in children with cerebral palsy. Perioperative management strategies, such as spinal cord monitoring, can decrease the number of complications post – surgery while infections can be treated with antibiotics or wound debridement. Most complications associated with NMS can be treated successfully and should not be the only deterrent for surgical intervention.
Failure to treat NMS can lead to long-term physical and emotional complications. The spine can become increasingly deformed, leading to heart problems and worsening lung function. Seating may become increasingly problematic to the point that it can no longer be corrected surgically while the deformity itself can become so bad so that it is no longer treatable for medical reasons as opposed to surgical reasons. Adequate emotional support for the child during all stages of treatment is essential.
Neuromuscular patients are challenging but good outcomes can be achieved through careful assessment, planning and by taking a multi-disciplinary approach. Due to the advancements of operative and peri-operative techniques, more complex cases with a significant number of co-morbidities are now seen as candidates for intervention. Depending on the stage of the deformity and the individual case there are various treatment options available which have been described in this article. These are all very well tolerated by the patient and can greatly improve their functionality and quality of life.